Introduction
Necrotizing fasciitis, often referred to as "flesh-eating bacteria," is a rare but serious bacterial infection. This infection affects the fascia, which is the connective tissue surrounding muscles, nerves, fat, and blood vessels. While rare, necrotizing fasciitis spreads quickly and can be life-threatening if not treated promptly.
This comprehensive blog post delves into the intricacies of necrotizing fasciitis, shedding light on its causes, symptoms, and available treatment options. We aim to enhance understanding of this severe condition, empowering individuals with knowledge to seek timely medical attention should they suspect its presence.
Causes of Necrotizing Fasciitis
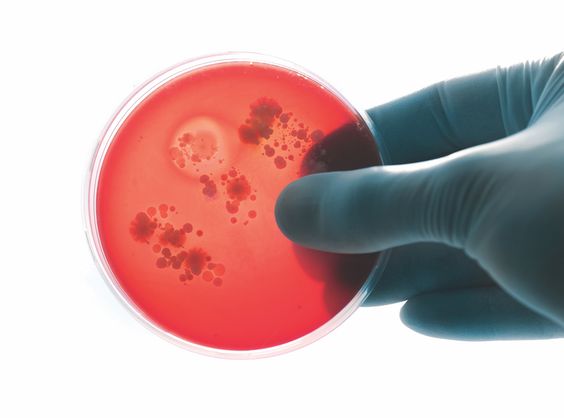
Necrotizing fasciitis arises from bacterial infection, most commonly by Group A Streptococcus (Streptococcus pyogenes), the same bacteria responsible for strep throat. Other bacteria that can cause this infection include:
- Staphylococcus aureus
- Vibrio vulnificus
- Escherichia coli (E. coli)
- Klebsiella
- Clostridium
These bacteria can enter the body through:
- Cuts, scrapes, burns, or insect bites
- Surgical wounds
- Puncture wounds
Symptoms of Necrotizing Fasciitis
Early symptoms of necrotizing fasciitis can be mistaken for other conditions, making early diagnosis crucial. These symptoms include:
- Redness, swelling, and pain at the site of infection, often extending beyond the initial area
- Intense pain that seems disproportionate to the visible injury
- Fever, chills, and sweating
- Nausea and vomiting
- Dizziness and confusion
As the infection progresses, symptoms worsen, leading to:
- Darkening of the infected skin, often with blisters or ulcers
- Skin becoming numb or tingly
- Foul-smelling drainage from the wound
Treatment of Necrotizing Fasciitis
Necrotizing fasciitis is a medical emergency that requires immediate treatment. Treatment typically involves:
- Intravenous antibiotics: High doses of potent antibiotics are administered to fight the bacterial infection.
- Surgery: The infected tissue is surgically removed to stop the spread of infection. In severe cases, amputation may be necessary.
- Supportive care: This includes managing pain, maintaining hydration and blood pressure, and providing oxygen therapy if needed.
Prompt diagnosis and aggressive treatment are crucial for survival. Early detection and intervention significantly improve outcomes.

.jpg)