Introduction:
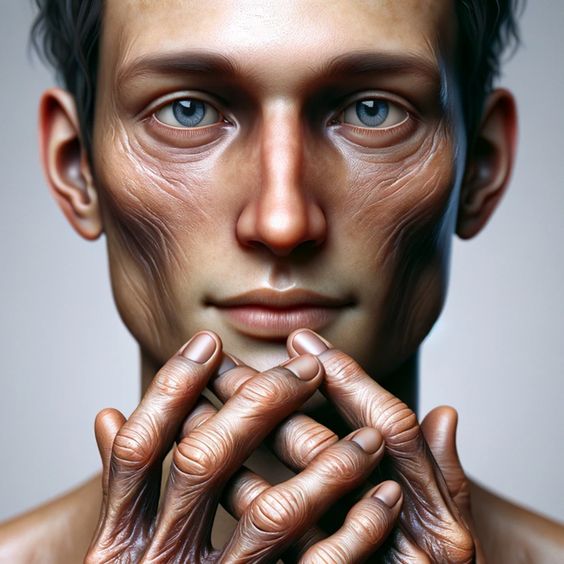
Scleroderma, also known as systemic sclerosis, is a rare autoimmune disease that affects the connective tissues. This chronic condition causes the body to produce an excess of collagen, leading to a hardening and thickening of the skin and internal organs. Scleroderma can present a wide range of symptoms and severity, varying greatly from person to person. While there is no cure for scleroderma, various treatments can help manage symptoms and improve quality of life.
Understanding the different types, symptoms, diagnosis, and treatment options for scleroderma is crucial for early intervention and effective management of the condition. This article aims to provide a comprehensive overview of scleroderma, empowering individuals to take an active role in their healthcare journey.
Types of Scleroderma:
Scleroderma is broadly classified into two main types:
1. Localized Scleroderma: This type primarily affects the skin and sometimes the muscles and bones. It generally doesn't involve internal organs. There are two main subtypes of localized scleroderma: * Morphea: Characterized by oval-shaped patches of hardened skin that may be discolored. * Linear scleroderma: Forms lines or streaks of hardened skin, often on the arms and legs.
2. Systemic Scleroderma: This type affects the skin and can also involve internal organs like the lungs, heart, kidneys, and digestive system. Systemic scleroderma further divides into two subtypes: * Limited cutaneous scleroderma: Skin thickening primarily affects the hands, face, and feet. * Diffuse cutaneous scleroderma: Skin thickening is more widespread, affecting larger areas of the body.
Symptoms of Scleroderma:
Scleroderma symptoms can vary greatly depending on the type and severity of the disease. Common symptoms include:
- Skin changes: Hardening, thickening, and tightening of the skin.
- Raynaud's phenomenon: Episodes of color changes in the fingers and toes in response to cold or stress.
- Joint pain and stiffness.
- Muscle weakness.
- Gastrointestinal problems: Acid reflux, difficulty swallowing, bloating.
- Lung problems: Shortness of breath, coughing.
- Heart problems: Irregular heartbeats, heart failure.
- Kidney problems: High blood pressure, kidney failure.
Diagnosis of Scleroderma:
Diagnosing scleroderma can be challenging due to the wide range of symptoms and its similarity to other autoimmune diseases. The diagnostic process often involves:
- Physical examination: Assessing skin changes, joint mobility, and other symptoms.
- Blood tests: Detecting specific antibodies associated with scleroderma.
- Imaging tests: X-rays, CT scans, or MRI scans to evaluate the extent of organ involvement.
- Biopsy: Examining a small sample of skin or affected tissue under a microscope.
Treatment for Scleroderma:
While there's no cure for scleroderma, various treatments help manage symptoms and prevent complications. The treatment approach is individualized based on the type and severity of the disease. Treatment options include:
- Medications: To suppress the immune system, improve blood flow, and manage organ-specific symptoms.
- Physical therapy: To maintain joint flexibility, improve muscle strength, and manage pain.
- Occupational therapy: To assist with daily activities and improve quality of life.
- Support groups and counseling: To provide emotional support and coping strategies.
Early diagnosis and proactive management are crucial for individuals with scleroderma. Working closely with a team of healthcare professionals can help individuals optimize their quality of life and minimize the impact of this chronic condition.

.jpg)